Trigger Finger
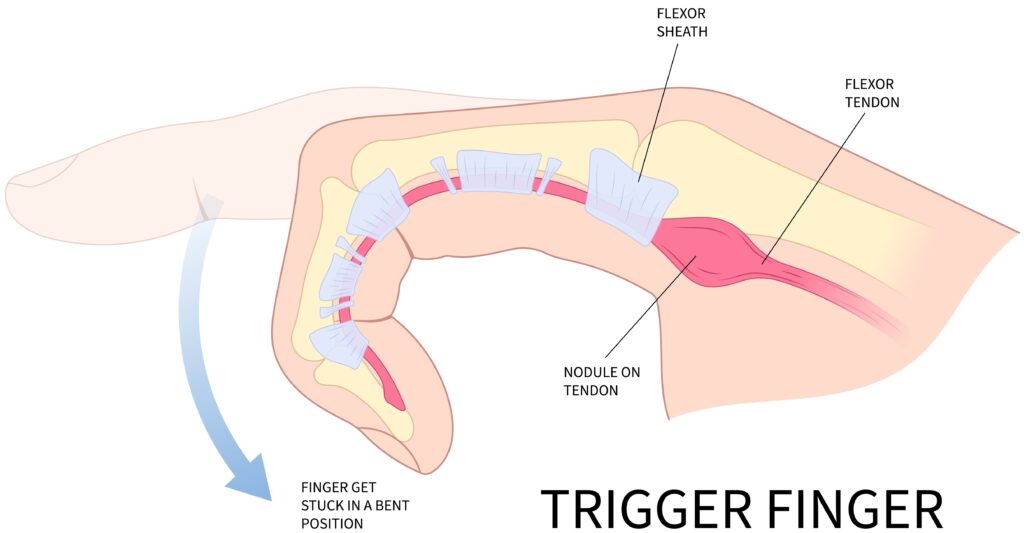
Trigger finger (or thumb) is a common condition where a finger catches, clicks or locks when bent or straightened. It occurs when the flexor tendon becomes irritated as it passes through a narrow pulley / tendon sheath in the palm. The condition can cause pain, stiffness and sometimes a visible or palpable “pop” as the finger moves. Treatment depends on the severity of symptoms and may include splints, injections, or minor day-case surgery.
Common Symptoms
- Finger or thumb that clicks, catches, or locks during movement
- Pain or tenderness in the palm at the base of the affected finger
- A lump or nodule that can be felt under the skin
- Stiffness, particularly in the morning
- Finger occasionally stuck in a bent position and needing to be straightened manually
Typical Causes
Trigger finger is caused by thickening or inflammation of the flexor tendon sheath. This narrows the space through which the tendon slides and causes it to snag as the finger moves. It is more common in people who perform repetitive gripping activities, in individuals with diabetes, and in association with inflammatory arthritis. It may also occur without any clear cause.
Seek urgent help if
You are unable to straighten your finger at all, if it becomes suddenly locked in a bent position, or if you develop redness, swelling or warmth over the tendon which may suggest infection or severe inflammation.
Call 999 for emergencies, or NHS 111 for urgent advice.
On this page:
Symptoms
Trigger finger can affect any digit but most frequently involves the ring finger, middle finger, or thumb. Patients often notice pain or tenderness in the palm over the base of the finger. The hallmark symptom is a clicking or popping sensation during flexion and extension.
At first, the finger may only catch occasionally, but as the condition progresses, it may lock completely in a bent position and require gentle force to release it. Morning stiffness is common, and symptoms may worsen after periods of rest. In some cases, a small, pea-sized lump can be felt in the palm corresponding to the thickened tendon sheath.
Causes / Risk Factors
Trigger finger occurs when the flexor tendon becomes inflamed or thickened at the level of the first annular pulley (A1 pulley) in the palm. This pulley acts like a tunnel that keeps the tendon close to the bone during movement. When the tendon cannot glide smoothly through the pulley, it causes friction and mechanical catching.
Risk factors include:
- Repetitive gripping or use of vibrating tools
- Diabetes mellitus (the most common systemic association)
- Rheumatoid arthritis or other inflammatory arthropathies
- Previous hand trauma or surgery
- Female sex and age between 40 and 70 years
Investigations & Diagnosis
Diagnosis is made clinically during examination. The key findings are pain over the A1 pulley and a palpable nodule that moves with the tendon. When the patient flexes or extends the finger, a characteristic click or “triggering” can be felt or seen.
Additional investigations may include:
- Ultrasound to confirm tendon thickening or exclude any other pathology
- Blood glucose testing if diabetes is suspected
Electrodiagnostic studies are not usually needed unless there are overlapping nerve compression symptoms (for example, coexisting carpal tunnel syndrome).
Treatment Options
Non-surgical
- Activity modification: reducing repetitive gripping or heavy hand use can lessen symptoms.
- Splinting: a finger or thumb splint can rest the tendon and may improve mild cases, particularly if worn overnight.
- Corticosteroid injection: the most effective non-operative treatment, relieving symptoms in about two-thirds of cases. It works by reducing inflammation in the tendon sheath. In diabetic patients, the response may be lower and blood sugar can rise temporarily.
Surgical
If triggering persists or recurs after injection, trigger finger release surgery may be recommended. This is a short, local-anaesthetic procedure performed as a day case. The surgeon releases the tight A1 pulley, allowing the tendon to glide freely again. The wound is closed with a few fine sutures and protected with a light dressing. Recurrence is rare.
Recovery & Follow-up
After injection, most patients experience improvement within a few days, though full benefit may take up to six weeks. Sometimes it feels like it hasn’t worked but then after a few weeks it stops catching. The finger can remain slightly sore at the injection site temporarily.
Following surgical release, gentle finger movement is encouraged immediately to prevent stiffness. Stitches are usually removed after 10–14 days. Most patients can drive within a few days and resume office-based work after one week, though heavy manual activity may need 3–4 weeks.
Follow-up ensures that motion has returned, pain has resolved, and there are no signs of infection or recurrence.
When to seek urgent help
You should seek urgent medical review if your finger becomes acutely swollen, red, or very painful after an injection or operation, as this may indicate infection. Inability to move the finger or new numbness should also be assessed promptly.
Call 999 immediately or attend A&E if you have a new injury with loss of movement or sensation in the hand, rapidly spreading redness or swelling with fever, or sudden severe weakness.
Use NHS 111 for urgent same-day advice if your symptoms are getting quickly worse.
If you’re experiencing trigger finger or trigger thumb, we can confirm the cause and tailor a plan – often starting with splints/hand therapy and exercises, with medicines, injections or surgery only where appropriate.
This page provides general information and is not a substitute for individual medical advice.
For emergencies (severe/new weakness, spreading infection, uncontrolled pain, significant injury) call 999, or use NHS 111 for urgent guidance.
Appointments:
- Self-pay patients can book without a GP referral
- Insured patients (Bupa, AXA, Aviva, Vitality, WPA, etc…) can book once authorised.
Clinics are available at:
- The Harborne Hospital – HCA, Birmingham
- Nuffield Health Wolverhampton Hospital
- The Priory Hospital, Birmingham
To book or ask a question, contact Vikki (Private Secretary):
☎ 07510 417479
✉ [email protected]