Tendon Injury (Flexor / Extensor)
Tendons connect muscles to bone, allowing the fingers and wrist to bend and straighten. A tendon injury occurs when one of these structures is cut, ruptured, or detached – often due to trauma such as a laceration or sporting accident. Flexor tendon injuries affect the palm side of the hand and prevent finger bending, while extensor tendon injuries affect the back of the hand and prevent straightening. These injuries require prompt specialist assessment and, in most cases, surgical repair followed by structured hand therapy for the best possible recovery.
Common Symptoms
- Inability to bend (flexor) or straighten (extensor) one or more fingers
- Visible cut or wound to the hand, wrist, or forearm
- Pain, swelling, and bruising
- Numbness or tingling if nearby nerves are involved
- Drooping of a fingertip or complete loss of finger motion
Typical Causes
Tendon injuries most often result from sharp lacerations, crush injuries, or sudden forceful trauma. Flexor tendon injuries commonly occur from knife or glass cuts, while extensor tendon injuries may follow minor lacerations over the back of the hand or sports-related impacts. Occasionally, the tendon may rupture spontaneously in patients with rheumatoid arthritis or degenerative changes.
Seek urgent help if
You cannot move your finger after an injury, have a deep cut to the palm or back of the hand, or experience numbness or loss of sensation. Immediate medical assessment is vital – delay can reduce the success of tendon repair and recovery.
Call 999 for emergencies, or NHS 111 for urgent advice.
On this page:
Symptoms
Flexor tendon injuries cause loss of bending at the finger joints. Patients often notice that one finger no longer curls-up when making a fist. The injury may be accompanied by a deep cut or open wound in the palm or wrist, and sometimes bleeding is minimal, masking the severity.
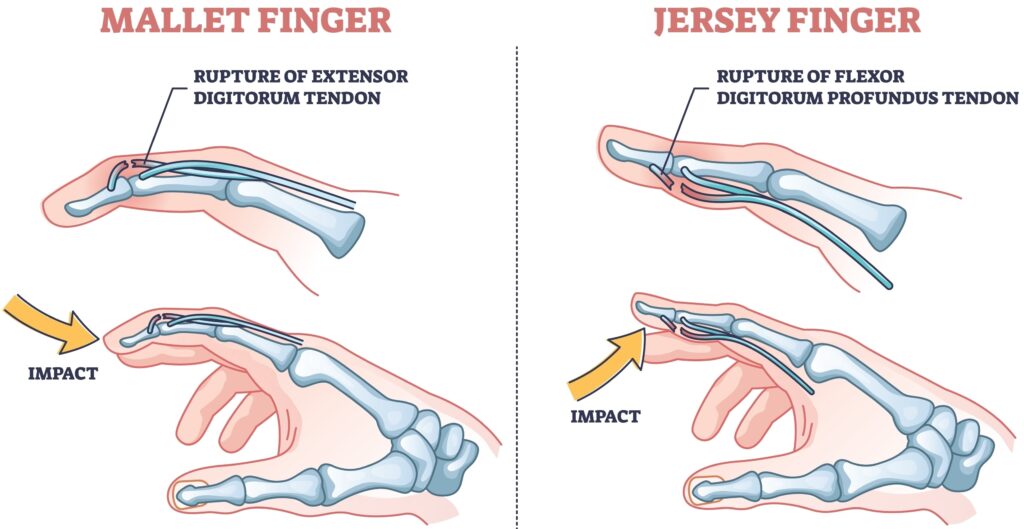
Extensor tendon injuries cause inability to straighten the finger or thumb. The finger may droop at one or more joints (for example, a “mallet finger” when the end joint cannot extend).
Both injury types produce pain, swelling, and tenderness. Numbness may occur if nerves are also damaged, and untreated tendon injuries lead to permanent loss of function.
Causes / Risk Factors
Tendon injuries occur when the strong fibrous cords that control hand movement are disrupted.
Common causes include:
- Sharp lacerations from knives, glass, or metal
- Crush or degloving injuries
- Sports injuries such as rugby, climbing, or skiing accidents
- Dog bites or industrial accidents
- Spontaneous rupture in rheumatoid arthritis or chronic tendon wear
Risk factors for poor healing include smoking, diabetes, delayed repair, infection, and poor compliance with postoperative therapy. Prompt specialist treatment gives the best chance of restoring function.
Investigations & Diagnosis
Diagnosis is made clinically by examining finger motion and assessing tendon continuity.
Typical findings include:
- Inability to actively flex or extend a finger
- Loss of tension when the tendon is palpated
- Abnormal posture (e.g. drooping fingertip or flexed finger)
Investigations may include:
- X-rays to check for associated fractures or foreign bodies.
- Ultrasound to visualise partial tears or locate retracted tendon ends.
- MRI for complex or delayed presentations.
Early recognition is key, as primary repair within the first few days produces the best outcomes.
Treatment Options
Non-surgical
Partial tendon injuries may sometimes be treated non-surgically with splinting and physiotherapy, but complete tendon ruptures almost always require surgical repair. Minor extensor injuries at the fingertip (mallet finger) can often be treated with continuous splinting for 6–8 weeks if the joint is stable.
Surgical
- Primary tendon repair: the standard treatment for most complete lacerations, ideally performed within 7–10 days of injury. The ends of the tendon are carefully stitched using sutures to restore continuity.
- Tendon grafting or transfer: used when the tendon is retracted, scarred, or previously ruptured.
- Skin or nerve repair: often performed at the same time if associated structures are injured.
Repairs are usually performed under regional anaesthetic using magnification for precision. Postoperative splinting and hand therapy are essential to prevent stiffness and ensure controlled movement.
Recovery & Follow-up
After tendon repair, the hand is immobilised in a protective splint – usually a dorsal blocking splint for flexor repairs – to protect the repair while allowing guided motion.
Rehabilitation is crucial and follows a carefully structured hand therapy programme:
- Early phase (0–4 weeks): controlled passive or limited active movement under therapist supervision.
- Intermediate phase (4–8 weeks): gradual increase in range and light functional use.
- Later phase (8–12 weeks): strengthening and return to normal activity.
Most patients regain good function, though recovery may take 3–6 months. Flexor tendon repairs are more technically demanding and slower to recover than extensor repairs. Long-term stiffness, reduced grip strength, or scar sensitivity are possible, but early and consistent hand therapy minimises these risks.
When to seek urgent help
You should seek urgent medical review if you develop new pain, swelling, redness, or discharge after surgery or splint removal, or if the finger suddenly “gives way” after a tendon repair, suggesting re-rupture. Inability to move the finger following an injury always warrants immediate assessment.
Call 999 immediately or attend A&E if you have a new injury with loss of movement or sensation in the hand, rapidly spreading redness or swelling with fever, or sudden severe weakness.
Use NHS 111 for urgent same-day advice if your symptoms are getting quickly worse.
If you’re experiencing a tendon injury or related symptoms, we can confirm the cause and tailor a plan – often starting with splints/hand therapy and exercises, with medicines, injections or surgery only where appropriate.
This page provides general information and is not a substitute for individual medical advice.
For emergencies (severe/new weakness, spreading infection, uncontrolled pain, significant injury) call 999, or use NHS 111 for urgent guidance.
Appointments:
- Self-pay patients can book without a GP referral
- Insured patients (Bupa, AXA, Aviva, Vitality, WPA, etc…) can book once authorised.
Clinics are available at:
- The Harborne Hospital – HCA, Birmingham
- Nuffield Health Wolverhampton Hospital
- The Priory Hospital, Birmingham
To book or ask a question, contact Vikki (Private Secretary):
☎ 07510 417479
✉ [email protected]